ASA Cycles

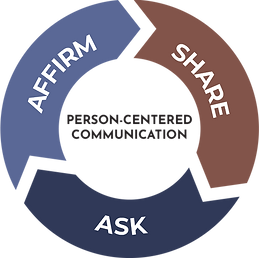
What are Affirm-Share-Ask (ASA) Cycles?
Providers use ASA Cycles as a simple way to remember and effectively apply communication and counseling skills that center patients during health care interactions. ASA Cycles expand on the Ask-Tell-Ask collaborative communication method that is widely applied in medicine and education and incorporate strategies shown to support health literacy and techniques from Active Listening and Adult Learning Theory.
ASA Cycles offer specific recommendations on “how to” operationalize respectful, efficient, person-centered care that supports patient autonomy. Using ASA Cycles repeatedly throughout conversations facilitates listening on the part of the provider, builds rapport and demonstrates that the provider is trustworthy. The patient actively participates in the discussion which is driven by their priorities and questions. The provider shares relevant health information in a way that is digestible,so the patient gets the information they need to make informed decisions and adhere to treatment plans.
Affirm/Acknowledge
When a patient shares something with you or asks a question, before responding with information, first affirm or acknowledge something about them or what they have said. This can be brief. There are various ways to affirm described below. By giving this acknowledgment, you are treating them as a person, whom you see and appreciate -- not just as a patient.
Useful Skills
Empathy
Empathy is caring about others feelings and experiences. This is integral to person-centered care. When showing empathy try using phrases that show you are trying to understand how someone feels like "Wow, that must have been difficult" instead of underplaying, falsely labeling their emotion, or already claiming to understand it.
Pointing Out Strengths/Positives
Most people are making efforts to improve their lives. One useful acknowledge skill is to acknowledge their own independent health efforts before providing information or possible corrections. This can look like, “I’m impressed that even with all of those challenges, you’ve been using a condom most of the time".
Validation
Validation can be used in conversations to let the person you are talking to know you understand where they are coming from. Using phrases like, "I here that all the time" lets the person know they are being reasonable and heard.
Body Language
Body language can convey a lot during a conversation. Things like maintaining eye contact, sitting at the same level, keeping a respectful distance, and nodding along convey attentiveness and care.
Finding Agreement
Instead of outright disagreeing or correcting people, try finding a part of what they said that you do agree with, identifying it and then going from there. This way people don't feel shut down and will be more receptive to new helpful information.
Share Content/Information
To make informed choices, patients need to have relevant, correct information about their options. This involves patient education during which patients obtain new relevant information that they will use when making decisions. For this process to be successful, the patient needs to have the new information integrated into their knowledge base.
Building Blocks of Learning

Learning requires integrating new information into an already present understanding of the world. This Integration requires that the person has:
-
heard the information (not always easy if they are distracted or anxious)
-
understood the information--which requires it to have been delivered in a language they speak, using terms they know
-
remembered the information
-
processed the information in order to recall it when needed
Visual/Tactile Aids

Visual/Tactile aids are a great way to help patients better understand what something is. Examples of these are sample IUDs (pictured to the left) or take home hand out sheets.
Using Plain Language
Numbers:
When describing relative risk; use common denominators instead of percentages. Instead of saying 0.3%, try saying "3 in 1000 people".
Phrases:
Make sure you are always using common language when talking to patients. For example, instead of saying "effectiveness", try saying "how well it works to prevent pregnancy". Instead of saying "bleeding profile", try saying "how your period comes".
Reflective Listening
Reflective Listening is when you are actively listening to what someone is saying and then are able to re-phrase it back to them in a way that shows you understand what they are saying. If you get it wrong then it offers an opportunity for the person talking to correct you which is a way for them to advocate for themselves and for you to have a better understanding of what they are telling you.
Ask A Follow Up Question
After sharing information with someone, try asking a follow-up question such as, "How would that be for you?" or "Has that ever happened to you before?" Ask questions that are open ended and encourage active participation. This provides an opportunity for people to integrate the new information.